Bristol City Council: local authority assessment
Overall summary
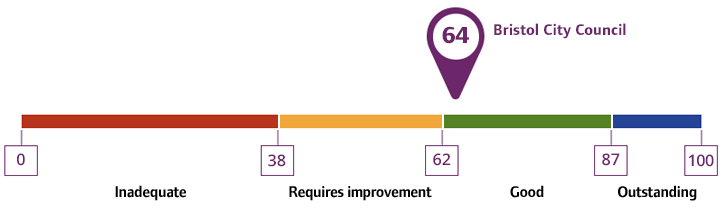
Local authority rating and score
Quality statement scores
Summary of people’s experiences
People’s experience of their assessment and care planning was mainly positive. They shared they felt listened to and involved in the planning of their care and support. Social workers took an approach considering the needs of the whole family. Staff used strength-based approaches and people shared experiences of how they were being supported to be as independent as possible. However, some people and unpaid carers shared there had been long periods of time between assessments and some care reviews.
Overall, the support provided by occupational therapy (OT) was praised by people and unpaid carers. One person told us their current OT was excellent, and had worked with them to consider adaptations that would meet their needs and keep them independent for longer.
People moving between services were mainly happy with the support they had received. A young adult moving to a residential college shared this had been a positive experience for them. Another relative praised the discharge process of their family member from hospital to rehabilitation, then back home, as having gone smoothly. In contrast, an unpaid carer explained that moving from children to adults’ services had been difficult in terms of the process. Partnership working was highlighted as being good between services. Although the sharing of information needed improvement, especially when people moved between health and social care.
Feedback from unpaid carers was more negative with many feeling their caring role was having a detrimental impact on their health and wellbeing. Respite options were currently more limited and unpaid carers felt having a short break was vital to be able to continue to provide good care. The process of assessments and reviews had taken too long for many unpaid carers along with delays with care starting.
Several unpaid carers told us direct payments had supported them in their caring role. People shared examples of how they were able to be creative in the use. For those not in receipt of direct payments, people told us they were aware of them but chose to receive care and support through a managed care package.
Summary of strengths, areas for development and next steps
The timeliness of assessment and reviews was improving after the local authority had taken a multi-pronged approach to address these, however, there were still further improvements required. Feedback from staff was improvements were also needed at the front door to the local authority, although some were underway. Staff worked in a strengths-based way and utilised systems to enable them to tell their story once. Improvements were underway to assessment times for unpaid carers alongside several other initiatives to provide support to them now and in the future. Advocacy was available to support people to contribute fully to care assessments, reviews and decision making.
Data provided by the Local Authority in January 2025 for care assessments showed a waiting list of 499 people. A shortage of staff was cited as the reason for the delays. Extra resources were now in place resulting in steady improvement with a 47% reduction since June 2024. For care reviews the waiting list was 1479 people, which was a reduction of 39% since January 2024. In terms of carers’ assessments, 326 unpaid carers were waiting in January 2025, and this was an increase from January 2024 where there had been 262 people waiting.
A range of work was undertaken across staff teams to prevent, reduce and delay people’s need for adult social care including occupational therapy support and provision of equipment and adaptations. Reablement services had been successful in supporting people and promoting independence. Work was underway to continue to improve usage of direct payments to give people more choice and control. People could access advice and information where needed, however, more work was being done to improve this, including a new directory of services. Some preventative projects were already in place, however, the local authority wanted to focus more on prevention in the future and partners agreed more could be done to further develop this area of work.
The local authority understood more work was needed to identify people who used services as well as those who did not through their data. Commissioners took positive steps to ensure providers considered people’s diverse needs and were culturally competent. Communities gave mixed feedback about working with the local authority, however there were some positive examples of working together well, such as working with the Somali community accessing direct payments. Feedback was that information provided by the local authority was accessible, however there were some areas which could still be improved.
Good relationships were evident with health, voluntary, community and social enterprise (VCSE) partners. Examples of strategic partnership working were given to areas such as the transfer of care hub with health partners. The partnership with mental health services was particularly highlighted as an area of focus and work was underway to implement a mental health hub to improve this further.
The local authority worked with local people and stakeholders using available data to understand the care and support needs of people and communities. Commissioning staff supported new and innovative approaches to care provision, which led to better outcomes for people. A key priority in Bristol was developing specialised housing for people with complex needs. The local authority had clear arrangements to monitor the quality and impact of care and support services and supported improvements where needed. Some care providers felt communication with the local authority had improved more recently and hoped this would be sustained.
Work had been undertaken to improve the process for young people transitioning to adult services, and feedback was this was making a positive difference to people and their families. Joint working with health partners in several areas was positive and this work continued to develop, for example with a new mental health integrated care team being established. Systems such as the emergency duty team worked well overall and work in relation to areas such as preventing provider failure was embedded with staff evidencing how they worked in person-centred ways to support people. Risks were managed by the local authority when a person moved out of the city to ensure relevant checks and communication had taken place. Access could be improved for staff in terms of having shared access to health partners IT systems.
Waiting lists for safeguarding were reducing due to a combination of factors including the introduction of a safeguarding hub. However, Deprivation of Liberty Safeguards remained an area where risks remained. Partners were positive overall in how safeguarding was managed by staff in terms of systems and processes, but there were areas for improvement needed in feeding back about safeguarding outcomes for people. The staff approach was person-centred and creative with people supported in the least restrictive way possible. A programme of work was underway to improve safeguarding which included the introduction of a new Multi-agency Safeguarding Hub and there was continued learning in relation to Safeguarding Adults Reviews.
A co-produced Vision for Adult Social Care had been developed to guide staff, along with a target operating model to improve systems, processes and how staff worked. A number of changes and improvements had been made as part of an ongoing transformation programme, for example, improving staff recruitment and retention, waiting lists and enhancing performance data. Senior leaders, staff and elected members on Policy Committees were committed to the changes underway whilst being aware of the challenges ahead.
There were many staff training and development opportunities, and we received positive feedback about these from staff. Some areas had been more recently developed by the local authority, such as the Interprofessional Practice and Competency Framework, whereas other areas were more established, such as the occupational therapy apprenticeship and social work assessed and supported year in employment (ASYE) programme. A co-production advisory group had been working with the local authority and were enthusiastic about their involvement in producing a co-production policy. The Technology Enabled Care team worked closely with staff and partners to support people with their care needs, safety and promoting independence. The local authority used feedback from people to improve service delivery. There were opportunities for staff to provide feedback to leaders in a number of ways.