Darlington Borough Council: local authority assessment
Overall summary
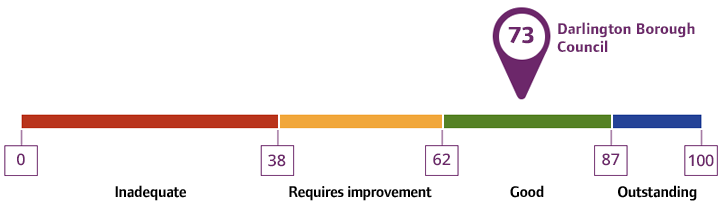
Local authority rating and score
Quality statement scores
Summary of people’s experiences
The local authority performed generally well compared to average in relevant published national data. For example, people felt they had more control of their daily lives and carers were more satisfied with social services than average.
Records and feedback from people showed generally positive strength-based approaches, involvement of the person receiving care and carers assessments with information advice and support. People said they were mainly happy with care provided. Evidence showed that people were generally involved in their care and support and given choice and control. Direct payments were higher than average which provided people with flexible and personalised services.
People’s feedback was also generally positive about their care and support and the choices available to them. Some carers said they were concerned about the support on offer post-19 following transitions of a young person to adult services.
Advocacy was more consistently offered and used to people going through a safeguarding process in the local authority than average and more people felt safe than national average.
Summary of strengths, areas for development and next steps
Darlington provided a good level of adult social care service and support. There was a consistent strength-based assessment programme with flexible approaches from staff as well as supportive management around support planning. Access to carers assessments were mixed, although once carers were identified they received a good level of support and national data was positive. A similar proportion of people to the national average had an annual review on time. There had been significant wait times for Care Act assessments and financial assessment wait times had also been long. The local authority said they had wrongly categorised people as waiting for a Care Act assessment and reduced the number of people they said had been waiting, providing a rationale after the site visit. Risk prioritisation was evident across all assessments and we did not see evidence of a negative impact of waiting.
There were good preventative measures in place with a Responsive Integrated Assessment Care team (RIACT), which provided a thorough assessment with very positive results. There were no delays to hospital discharge and the data around reablement and outcomes following discharge were better than average. The local authority had a ‘Making Every Contact Count’ approach, with effective community support. There was a housing approach to avoid residential care and a flexible approach to using extra-care for people. Although there were some delays to occupational therapy assessments and adaptations.
There were some shortfalls around the collection and systematic use of equality data, coproduction was in its infancy and feedback about accessible information in different formats was mixed. The local authority had clear plans to further embed public health approaches in its adult social care work to address health inequalities.
There was good partnership working in the discharge of the better care fund and work had been done to address gaps in the care market. There was also a good quality assurance support service from the local authority and additional funding had been provided to support the home care market. Although we heard about some concerns around a lack of post-19 educational and day services.
Collaborative working with partners was evident, particularly in relation to hospital discharge and the interface they had with social work teams. Section 75 agreements worked well with co-location and multidisciplinary team working embedded. Academic work undertaken with the university was brought back by social workers into practise. The local authority commissioned the voluntary community and social enterprise sector to provide services to support people in the community and there were market engagement sessions which fostered a positive relationship with providers.
Out of hours systems were robust with people having access to respite in an emergency. Right Care Right Person methodology supported staff to act without having to rely on partners. There were effective hospital discharge arrangements and there was mostly positive feedback about transitions to adult services.
Safeguarding arrangements were effective and proportionate to the size of the local authority and involved shared arrangements with the children's safeguarding board. There was a good performance on deprivation of liberties assessments and good oversight of decision making of the S42 threshold, via a dip sampling method.
We found open and transparent relationships with senior leaders and staff felt they had the ability to challenge and influence policies and practice. Leaders had an impact on staff retention, and we heard reports of a positive workplace culture. A key feature of the work of leaders in recent years, had been to embed practice and validation forums. These effectively supported staff learning. The local authority demonstrated a commitment to continuous learning related to cultural needs and commissioned external training.